Our body’s largest ball-and-socket joints
The hip joints are the largest ball-and-socket joints in the human body. The hip socket and the head of the thigh bone (femur head) are connected by the hip joint. Half of the femoral head is surrounded by the hip socket. This provides the hip joint with good, bony stability. This stability is additionally supported by a cartilage seam, a joint lip.
Along with the lower back muscles, the hip muscles in the hip and thigh area provide stabilisation, absorb shocks and bring the knees and feet into correct alignment. With its partner, the lower back, the hips literally play a pivotal role in nearly all physical activities.
With every step we take, our hip joints must bare loads of several times our body weight. When climbing stairs, for instance, the hips bare pressure of almost three times our body weight. While the load is particularly high in sports such as running or jumping, it is much lower in others, i.e. cycling or swimming.
Range of treatments: The hips
- Arthrosis
- Hip pain
- Hip fractures
- Impingement
Special pathologies affecting the hip joint
Arthrosis of the hip joint
Arthrosis is a progressive wearing down of the articular cartilage, which may occur naturally due to aging but may also be caused by injuries or congenital malformations. In the process, the joint surfaces are gradually destroyed and typical complaints such as pain during the first few steps after inaction, night pains as well as restricted movement begin to arise.
History
The first attempts to implant an artificial hip joint date back to 1821. A wide variety of materials have been tested since that time. It was not until 1959/60 that Sir John Charnley introduced bone cement and used a plastic (polyethylene) piece as a sliding partner for the prosthesis. Since then, the basic features of hip arthroplasty have remained the same. Advances in understanding of friction, materials research, biomechanics, and surgical techniques have led to significant improvements in implant tolerability and longevity. Today, for example, about 95 out of 100 hip prostheses are still intact after 20 years.
Causes
- Mechanical causes (malpositions)
- Accidents (hip fractures)
- Circulatory disorders (avascular necrosis, Perthes disease
chronic polyarthritis)
Symptoms
- Pain in the first few steps, night pain
- Exertion and rest pain in the groin, buttocks, thighs
- Increasingly limited range of movement
- Limping
Risk factors
- Weight not born correctly
- Genetic influences
- Obesity
Treatment options
Surgical technique/access to the hips
There are different surgical approaches to accessing the hip, each of which has advantages and disadvantages. One of the great challenges for the surgeon is to be able to see the joint well and completely in order to have sufficient space for inserting the implants. Another challenge is to optimally preserve or retain the existing capsular tissue and musculature and to protect the surrounding nerves and blood vessels. In principle, the implantation of an artificial joint is either done with or without cement. During hip replacement surgery, we use almost exclusively cement-free implants.
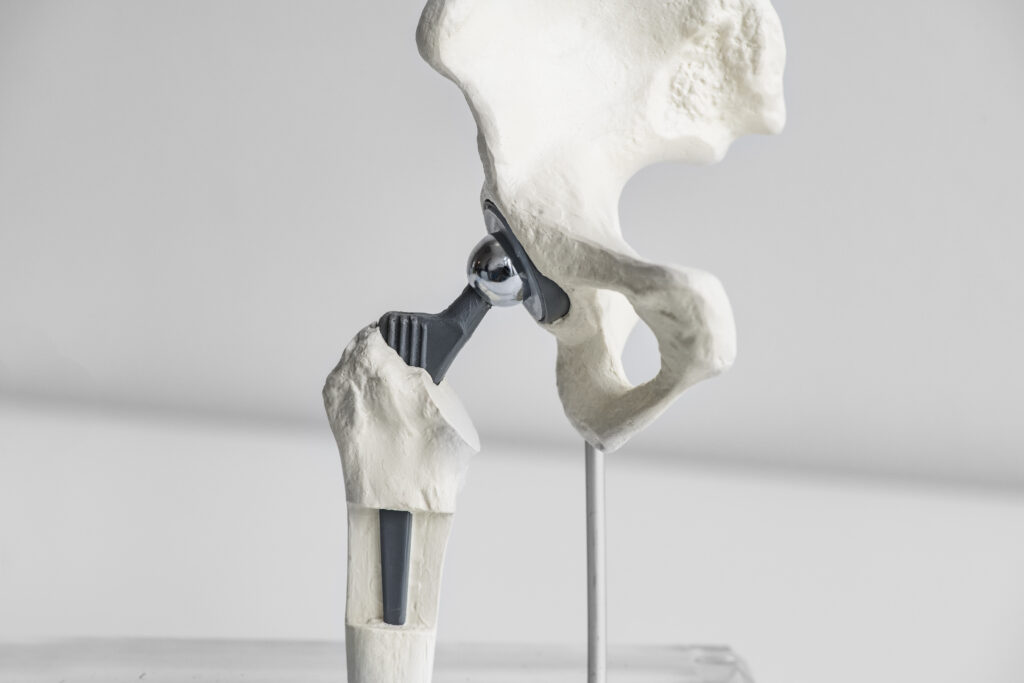
Components of the hip prosthesis
Modern artificial hips are modularly constructed from several components made of different materials. The stem, which is inserted into the femur, and the cup, which is anchored in the pelvis, are made of titanium. The prosthesis head is made of ceramic while the the liner for the cup is made of polyethylene or ceramic. On the one hand, this enables customised adaptation to the patient’s anatomy and, on the other hand, keeps the friction of the materials to a minimum.
After surgery
Patients with a new hip can typically put weight on their new hip using crutches the day after surgery. The hips are generally ready to bare full weight after three to four weeks, provided that the individually tailored aftercare plan is followed. Typically, an inpatient stay usually lasts seven to ten days. Afterwards, either an outpatient physiotherapeutic follow-up or a follow-up stay in one of the rehabilitation centres is highly recommended. Hip operations are associated with a considerable risk of thrombosis, which is why preventative administration of a blood-thinning medication (thrombosis injection) is indicated for a period of five weeks. In addition, we recommend wearing compression stockings.
Physical activity & sport
Sport contributes greatly to overall wellbeing. Naturally, however, the increased demands on the body resulting from sport can wear down the prosthetic components. Nevertheless, studies have shown that improving strength and coordination through exercise has a positive effect on the longevity of an artificial joint. Most sports that could be enjoyed safely before surgery can also be enjoyed with an artificial hip joint. However, sports that require a high degree of running and jumping (e.g. football, basketball, running) should be avoided.